What Is Dupuytren’s Disease?
This article explains what is Dupuytren’s Disease caused by and how it’s diagnosed and treated.
Dupuytren’s disease (also called Dupuytren’s contracture) was first described in 1831 by Baron Guillaume Dupuytren, a celebrated French surgeon. Thus, the name Dupuytren’s contracture became associated with this malady. It is a condition most commonly seen in patients of northern European ancestry, though it can be seen in patients of all races.
There is a strong familial tendency to develop Dupuytren’s disease, making it believed to be a genetic disorder. However, the actual gene(s) involved have not been determined, and some patients have no known affected relatives.
What Causes Dupuytren’s Disease?
The exact cause of this process is unknown. It may be seen with other connective tissue diseases (bursitis, arthritis, tendinitis, etc.). While the development of Dupuytren’s cords or nodules may occur following trauma or surgery, the exact relationship is uncertain.
What Are the Signs and Symptoms?
The Nodule
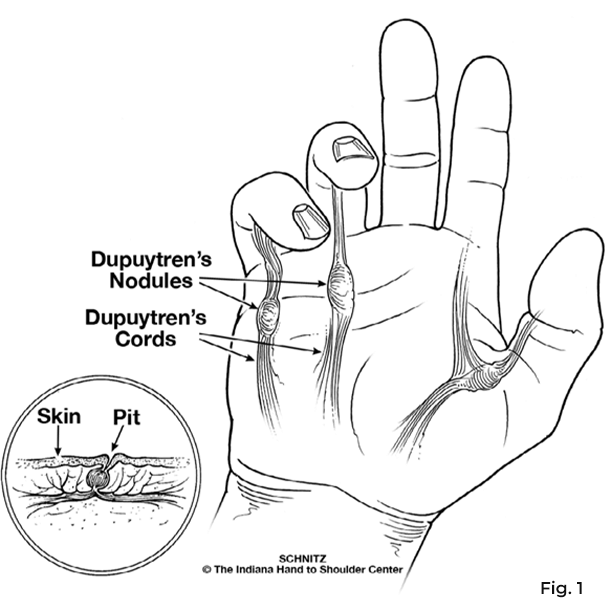
The most common evidence of the disease is a “lump” or nodule in the palm near the flexion crease, most often located at the base of the ring or little finger. This lump or nodule may also occur at the base of the thumb. (Fig. 1)
Although the appearance of these nodules in the finger usually occurs within the course of the disease, these nodules may be evident as the very first symptom.
The Pit
Another sign or symptom of Dupuytren’s contracture is known as a dermal pit. The pit may be single or multiple and appears as a small, local, deep indentation of the skin. This may be the first finding, it may come later, or the pit may never appear at all.
The pit is usually in the palm but can also be found in the fingers. This indentation occurs as the normal fibrous bands that hold the palmar skin in place shorten, drawing the attached skin deeper than the surrounding skin.
The Cord
The cord is a longitudinal fibrous band that extends from the palm into the finger(s). It most often appears with a nodule, but it can be separate. It may appear as a single or multiple bands.
The cord or band creates a flexion contracture at the finger joints as it crosses the joints; in other words, the cord pulls the finger into a bent position. Once the contracture has started, the process may proceed (either slowly or rapidly) to a severe deformity of one or several fingers. Even if only one or two fingers are involved, this condition may become so advanced that daily activities are embarrassingly awkward.
The ring and small fingers are the most frequently affected. The long finger is next, followed by the thumb. The index finger is seldom involved.
What Is the Nature of the Disease?
- The process is not malignant.
- The disease may progress slowly or have periods of temporary arrest or rapid progression.
- Involvement of the feet may be associated in 15-20% of cases. Other body parts may also be affected. Involvement of the disease in both hands is common.
- Flexion contractures usually occur at either of the first two finger joints.
- Flexor tendons are never involved in this process.
- Skin may be involved by the infiltration of dermal layers with the disease.
- This condition is not painful, except for tenderness in the area of infiltration or during an inflammatory phase.
- Recurrence is frequent, particularly at the proximal interphalangeal joints.
How Is It Treated?
The aim of surgery in Dupuytren’s contracture is to regain maximum hand function rather than totally cure the disease. If there is no present deformity and no loss of hand function, surgery may be delayed until significant deformity has developed.
Therefore, the small palmar nodule rarely requires surgery unless it is sufficiently tender to interfere with activities.
A progressive contracture is an indicator for surgery and is best demonstrated when the hand can no longer be placed flat on a tabletop. There is sufficient deformity to demonstrate that hand function will eventually be threatened at this stage. (Fig. 2)
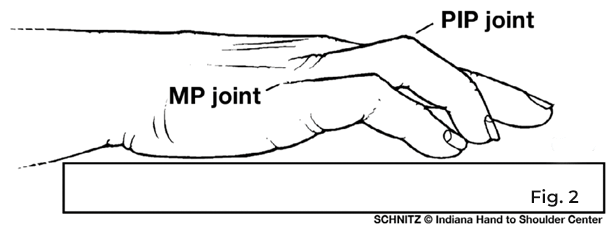
A flexion deformity at the first finger joint (MCP) is usually correctable with surgery. A deformity at the second finger joint (PIP) is not always correctable and recurs more frequently. Your physician will be able to discuss your symptoms and a possible prognosis.
What Is the Surgical Procedure?
Subtotal palmar fasciectomy is the surgical removal of the taut, contracted palmar fascia from the palm and afflicted finger(s). The amount of time spent during the operation depends on the amount of involvement, but surgery generally requires one to three hours. Surgery is usually performed under a regional anesthetic.
A zigzag incision is made in the palm and may be extended into the finger(s). Because it is crucial to protect the nerves and blood vessels of the palm and fingers, meticulous dissection by the surgeon is necessary.
Because of the type of incision, numerous “stitches” are required for adequate closure of the wound. Drains may be inserted to provide maximum drainage from the hand and are usually removed the first or second day after surgery. Occasionally, the surgeon may elect to leave part of the surgical wound open to prevent complications. In this instance, the incision heals naturally, and stitches are not required.
Following surgery, the hand is wrapped and immobilized in a large “boxing glove” type bulky compressive dressing, which is generally removed three to five days following surgery. The surgical wounds may be slow to heal and may occasionally gap open during rehabilitation. The physicians and therapists will monitor this closely to balance the program of wound care, exercise, and splinting.
Other techniques used to treat Dupuytren’s are limited fasciotomy and dermofasciectomy. Limited fasciotomy is a minimally-invasive surgery where a small section of the diseased cord is removed. It is often done under a local anesthetic. Dermofasciectomy is most commonly done for patients with recurrent disease in a finger previously operated on. It involves not only the removal of the diseased fascia but also the overlying skin to try to prevent further recurrence.
What Are the Post-Operative Considerations?
Post-operative therapy appointments will be made for periodic checks on your healing progress. Your therapist will provide you with a specific exercise program. Discomfort with early therapy is not uncommon, but this improves with time. Several months of therapy may be required to regain joint mobility. Some residual inability to fully extend the involved fingers is common.
Skin incisions may remain large and somewhat tender for several months but will gradually improve. Splinting the involved fingers to prevent the recurrence of contractures may be necessary (usually at night) for six to nine months following surgery. The goal of surgery is to remove the diseased tissue and prevent further contracture. Full return of finger function is not always possible, and, in some cases, the deformity may reoccur.
New Treatments
Newer, less invasive treatments for Dupuytren’s disease are available. Benefits may include less recuperation time, less discomfort, and quicker resumption of normal activity. Because these less invasive treatments do not actually remove the diseased tissue, recurrence rates may be higher than with more traditional surgery.
Needle aponeurotomy is an alternative to open surgical procedures. This old surgical technique was abandoned for many years but has been practiced and perfected by a group of French surgeons for about 30 years. It has been practiced in the United States since 2003.
The technique is performed on an outpatient basis and involves administering a small amount of local anesthetic in multiple locations around the diseased tissue without any skin incisions. A fine hypodermic needle divides the cord in multiple locations, allowing the finger to be immediately extended.
Typically, patients wear band-aids for about 24 hours and resume their normal activities within a few days, without the need for any formal post-operative splinting or therapy.
The newest option is the only FDA-approved nonoperative treatment called collagenase injection. It is an office-based procedure where a mixture of enzymes is placed into the diseased tissue. The enzymes work by dissolving the fibrous cord causing the contracture. Once the enzyme has had time to weaken the cord, typically by the following day, the finger is manipulated so that the cord will rupture and the finger can be straightened.
Typical side effects may include bruising, swelling, and soreness at the injection site. No formal therapy is required, although a hand-based splint is prescribed for night use. Most patients resume normal use of their hand within days, though forceful grasping should be avoided for two and four weeks.
No part of this work may be reproduced without written permission from the Indiana Hand to Shoulder Center.
Disclaimer: The materials on this website have been prepared for informational purposes only and do not constitute advice. You should not act or rely upon any medical information on this website without a physician’s advice. The information contained within this website is not intended to serve as a substitution for a thorough examination from a qualified healthcare provider. The display of this information is not intended to create a health care provider-patient relationship between the Indiana Hand to Shoulder Center and you.
Dupuytren’s Disease Patient Handout

